In honor of International Women’s Day, we look at the cancer that is the second leading cause of cancer death in women: breast cancer.
There are different types of breast cancer, but they all correspond to the disease in which cells in the breast multiply out of control. This can result in the formation of a lump or mass. Breast cancer can spread outside of the breast, going through blood vessels and lymphatics to go to nearby lymph nodes or other organs (such as the liver, lung, brain, or skin). This is called metastatic disease.
Symptoms
The most obvious symptom of possible breast cancer is the formation of a new lump or mass in the breast or under the arm, in the axillary (armpit) area. The emphasis is on a new lump, as there are other more common causes of benign lumps in the breast, such as fibrocystic changes, that can make it feel tender and sore. This usually depends on a woman’s menstrual cycle.
Nevertheless, there are other possible warning signs of breast cancer. These include:
- Thickening or swelling of an area in the breast
- Redness or dimpling of breast skin (the skin looks like an orange peel)
- Pain in any area of the breast
- Changes in the size or shape of the breast
- Nipple discharge other than breast milk (e.g. blood)
- Nipple retraction or inversion
Some of these symptoms may be for other reasons aside from cancer, but this only highlights the necessity of seeing your doctor for some diagnostics. The inverse is also true: sometimes, breast cancer does not have any symptoms at all. This is particularly important in the early stages: during which it can be most difficult to catch the disease is when it is best to treat it, as the prognosis is always better when intervention is done at an early stage.
Should you also have some constitutional symptoms, such as unintentional weight loss, it is also best to seek medical consult.
Risk factors
Risk factors are characteristics in your lifestyle, personal history, and family history that may make you more susceptible to developing breast cancer. Some of the risk factors are changeable; if you alter certain lifestyle choices, for example, you can reduce your risk of disease. On the flip side, there are also those that you cannot change.
There’s no need to fret if you have the risk factors mentioned here. Not all of the risk factors have the same effect, and just because a woman has one (or more) of the risk factors, it doesn’t mean that she will develop breast cancer with certainty.
- Age – Increasing age is a risk factor for most types of cancers, breast cancer included.
- Genetic mutations (BRCA1 and BRCA2) – This familial genetic mutation increases the risk of both ovarian and breast cancer.
- Early menarche (starting menstrual periods before 12 years of age) and late menopause (after age 55) – This increases a woman’s exposure to estrogen, which is implicated in the development of breast cancer
- History of breast cancer or other breast diseases – Recurrence of breast cancer is possible. Previous diagnoses of atypical breast lesions also increase the chances that these previously non-malignant lesions.
- Family history of breast or ovarian cancer – First-degree relatives or having multiple family members from either the paternal or maternal side who have breast cancer is a strong risk factor.
- Lifestyle factors – As with most diseases, being overweight or obese, not having enough physical exercise, and drinking alcohol increases the risk.
- Hormones and reproductive history – Women who take either some oral contraceptives or take hormone replacement therapy during menopause can increase their risk for breast cancer, especially when the latter is taken for more than five years. In addition, having a first pregnancy after 30 years of age, not breastfeeding, and never having a term pregnancy are additional risk factors.
Knowing these risk factors are important, so you can take what are changeable and make healthier lifestyle choices.
Self-Examination
Women are also advised to regularly do a self-examination of their breasts to feel for any new lumps or masses and to seek consult when this happens.
Screening
Risk factors or no, it is important for women aged 50 to 74 years old to get regular breast cancer screening. These are current recommendations; however, women younger than 50 years old who have strong risk factors as aforementioned may be screened earlier, depending on physician’s advice.
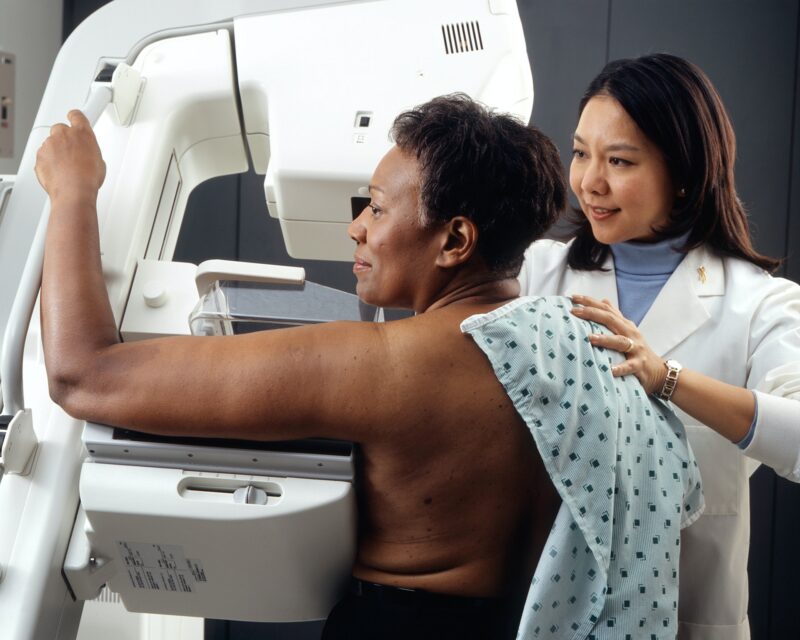
Breast cancer screening refers to the conduct of diagnostics regularly, before a woman has any symptoms, to catch the disease at an early stage. The recommended screening tool is a mammogram, which allows for radiographic visualization of breast tissue. Through this, doctors can check the breast and nipple area for masses, thickened tissue, and calcifications. If there are any findings, an ultrasound guided biopsy can be arranged. If the mammogram is normal, continued screening as per guidelines is done.
Mammograms involve standing in front of the machine, and you will be required to press your breast on a plastic plate while the image is being taken. This is done to take both frontal and lateral views of the breast. Most women find it uncomfortable and even painful, although it only lasts a few seconds. It is advised that mammograms not be done around the time of your period, as this time tends to make the exam more uncomfortable.
Sometimes, during screening, mammograms can detect lesions that are not actually cancers. This is called a false-positive result, and it can cause much anxiety for patients. Mammograms can also miss some types of breast cancers, and this is called a false-negative result. Sadly, this may delay diagnosis and treatment.
Diagnosis and treatment
Mammograms are also used for the diagnosis of breast cancer and, if there is a lesion suspected, a biopsy is done afterwards.
Biopsies are performed using small needles to extract some of the suspicious tissue in the breast. These tissue specimens are then submitted for a pathologist to examine under the microscope to check if the lesion is benign or malignant and, if malignant, describe how bad it is. Based on this, the clinicians and surgeons can come up with a treatment plan that may include surgery, radiotherapy, hormonal therapy, biological therapy (such as immune modulators), and/or chemotherapy.
If breast cancer is diagnosed, additional tests are done to check if the cancer has spread throughout the body. This process is called staging and is also important in the development of a treatment plan.
How we can help
Whether you or your loved one needs help going to medical appointments, postoperative or therapeutic care, or with medication management, Likas Nursing and Home Care can help you. We can create a care plan that is personalized for your needs and is in collaboration with the rest of your health team. Contact us today!



